Lung cancer screening: diagnosis in the nick of time
Lung cancer is the leading cause of cancer mortality worldwide. Only 16 % of patients survive for 5 years, compared to 89 % with breast cancer and almost 100 % with prostate cancer. Likewise, only 16 % of patients with lung cancer are diagnosed before the disease has spread (vs. 60 % with breast cancer and 90 % with prostate cancer). “Once symptoms develop, it is too late”, emphasised Giulia Veronesi, MD, Division of Thoracic Surgery, European Institute of Oncology, Milan, Italy.
In contrast to breast and prostate cancer, identification of early lung cancer is not part of established screening programmes. As Dr. Veronesi noted, screening with low-dose computed tomography (LDCT) should be urgently implemented in Europe. LDCT has been shown to be superior to X-rays for the detection of NSCLC. “It is a non-invasive tool, and the examination can be performed quickly and at low cost, without the use of contrast medium.”
Lung cancer mortality is reduced by LDCT screening, as surgery then offers the prospect of cure in an earlier stage. The 10-year survival rate for resected stage I cancer is as high as 92 % [1]. “Diagnostic algorithms allow for a safe screening process and low numbers of resections for benign disease”, stated Dr. Veronesi. In a study on the distribution of lung cancers according to volume doubling time, 10 % of screened tumours were overdiagnosed, meaning that these tumours grew so slowly that they would not have affected the life expectancy of the patients, as they showed a volume doubling time of more than 600 days [2]. Optimal selection of the high-risk target population and correct screening intervals can be achieved by use of validated risk models. Also, cost-effectiveness of lung cancer screening has been established: “These costs are lower than those of breast screening.”
Large-scale assessment of early detection
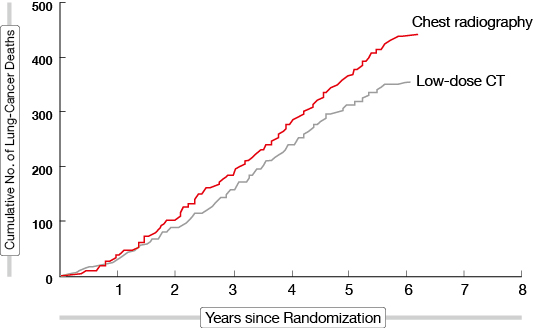
A number of cohort studies have investigated the usefulness of screening, including the Early Lung Cancer Action Program, the Anti-Lung Association Project in Tokyo, Japan, the Nagano Population-Based Lung Screening Trial, the NELSON Trial, the Italian Lung Cancer CT Screening Trial, the Multicentric Italian Lung Detection Trial, the German Lung Cancer Screening Intervention Study, the Danish Lung Cancer Screening Trial, and the United Kingdom Lung Cancer Screening Trial. In the US, the National Lung Screening Trial was the largest randomised controlled trial of LDCT screening for lung cancer (n = 53,454) [3]. People with high risk for lung cancer were randomly assigned to undergo three annual screenings with either LDCT or chest radiography. The trial achieved its goal of showing that the stated mortality reduction threshold of 20 %, which was required to provide national screening, was reached with LDCT as compared to radiography (Figure). “The results led to the acceptance of screening in the US,” noted Claudia Henschke, PhD, MD, Head of the Lung and Cardiac Screening Program, Mount Sinai Medical Center, USA.
Figure: Lung-cancer-related mortality after radiographic versus low-dose computed tomography screening in the National Lung Screening Trial
Aggressive smoking cessation programmes increase the effectiveness of screening and should therefore be fully integrated into all screening programmes. This implies that optimum smoking cessation techniques must be identified. Also, registries are needed for continued improvement and quality assurance. “More nimble methodology for assessing new potential screening tests is called for”, said Dr. Henschke. Collection of biological samples (blood, sputum, urine, buccal cells) for future integration into screening is important.
Source: Special Session: Lung Cancer Screening and Prevention, 26th September, 2015
REFERENCES
- International Early Lung Cancer Action Program Investigators, Survival of patients with stage I lung cancer detected on CT screening. N Engl J Med 2006; 355: 1763-1771
- Veronesi G et al., Estimating overdiagnosis in low-dose computed tomography screening for lung cancer: a cohort study. Ann Intern Med 2012; 157: 776-784
- The National Lung Screening Trial Research Team, Reduced lung-cancer mortality with low-dose computed tomographic screening, N Engl J Med 2011; 365: 395-40