The clinical care pathways in early-stage lung cancer are changing
Jessica Donington, MD, MSCR, Section Thoracic Surgery, The University of Chicago Medicine, Chicago, USA
Which agents that are currently being investigated in the neoadjuvant setting in patients with resectable NSCLC look promising from the present point of view?
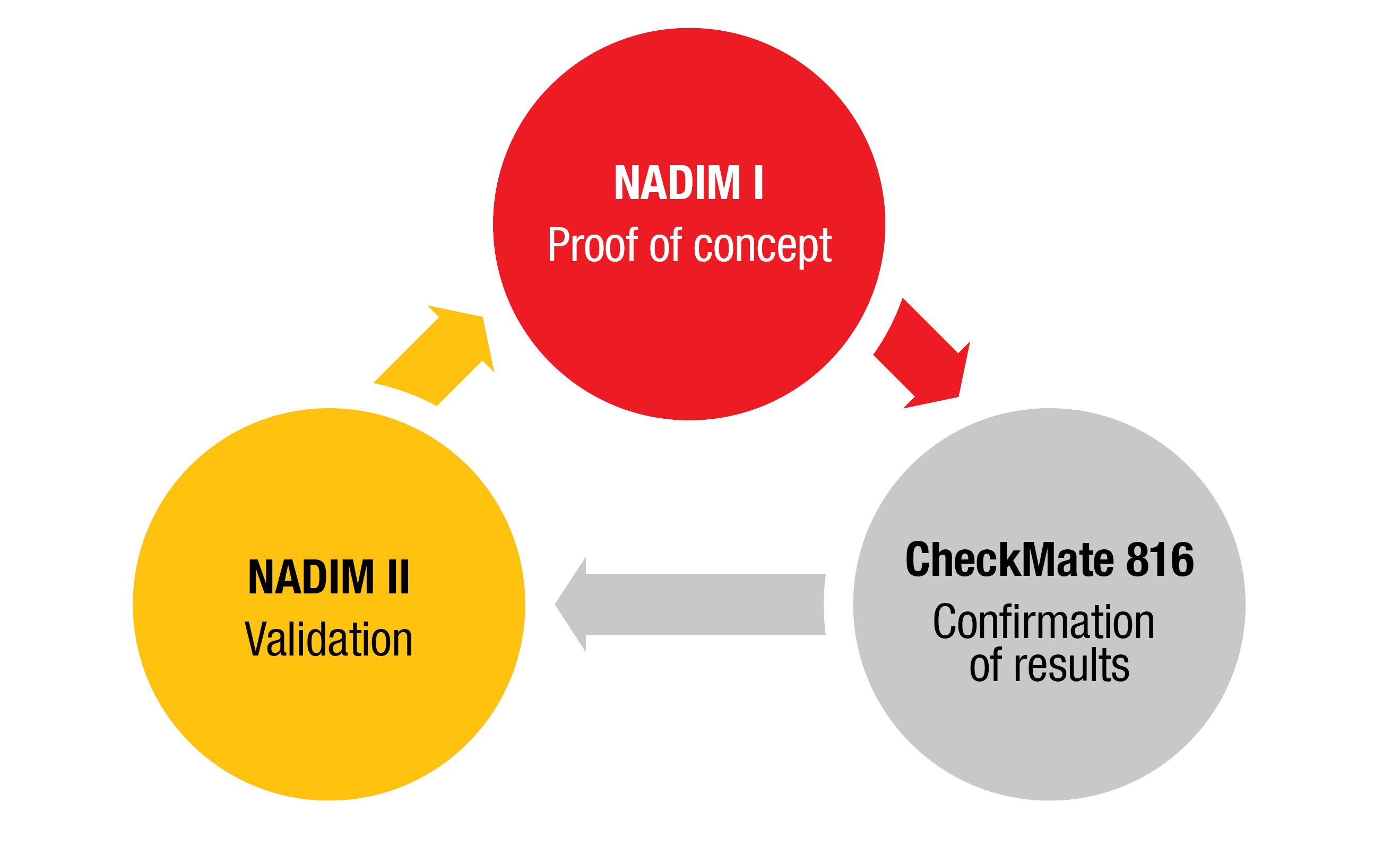
Many immunotherapies are being studied in the neoadjuvant or perioperative setting, but the only one that has been reported in a phase III trial as neoadjuvant treatment to date is nivolumab. There are three prospective trials that assessed nivolumab in the resectable setting. The NADIM I trial was a groundbreaking phase II study that looked at nivolumab plus chemotherapy followed by resection and demonstrated impressive results regarding pathologic endpoints and two-year survival [1]. It was followed by the first phase III trial evaluating chemoimmunotherapy, the CheckMate 816 study. The addition of nivolumab to 3 cycles of chemotherapy led to dramatic improvements in the pathologic complete response (pCR) rate, major pathologic response rate, and event-free survival [2]. Key surgical outcome data from CheckMate 816 that were presented at last year’s ASCO Congress were important, as this treatment needs to be demonstrated to be safe with respect to surgery [3]. The findings reported by Dr. Spicer gave us the impression that nivolumab plus chemotherapy can indeed be administered safely, with no increased morbidity or mortality compared to induction chemotherapy alone.
The final bit of prospective data that was presented this year at ASCO was the randomized phase II NADIM II trial. It included approximately 100 patients randomized to either 3 cycles of paclitaxel/carboplatin or paclitaxel/carboplatin plus nivolumab. The pCR rate was significantly improved with the addition of nivolumab [4]. Across these three trials, the pathologic results line up very nicely (Figure). I think it is important that we now have three trials conducted in a prospective setting all of which used similar induction agents, obtained similar pathologic response rates and had similar short-term surgical outcomes. Now we are waiting for the survival data.
Another nice aspect of these trials was that PD-L1 staining in the tumor seemed to be predictive in all three trials. There was some increase in the pCR rate compared to chemotherapy alone in PD-L1–negative patients, but the rates were definitely higher in the PD-L1–positive population and even higher in the PD-L1–high expressors. It is nice to see a biomarker that behaves consistently in this setting.
How does the intensity of neoadjuvant treatment affect patient outcomes?
I do not know if “intensity” is the right word when talking about neoadjuvant treatment. We think that the effect of neoadjuvant chemotherapy or radiation therapy may depend on the number of cycles or the dose. Adding radiation to chemotherapy is known to produce higher pCR rates, which can be further increased by augmented radiation doses or additional doses of chemotherapy. In this new treatment paradigm with immunotherapy, which is a whole new class of agents, nobody actually knows how many doses need to be given.
The randomized phase III neoSCORE trial conducted at a single institution in China assessed if the number of neoadjuvant chemotherapy cycles (i.e., 2 vs. 3) matters [5]. Unfortunately, the study was closed early, but the findings indicated improved pCR rates with 3 cycles, although one can question if it is the additional dose or simply the additional time from initiation of therapy that affect the pCR rate. We believe that these medications retrain the immune system and therefore may continue to work long after the resection has been performed. Therefore, it is hard to know how many doses should be administered. While we use pathologic endpoints to guide some of our decisions, this is a new class of medications, and pCR may not be the only indicator for overall response. Nevertheless, we are starting to question how many is enough. The upcoming series
of worldwide trials evaluating perioperative chemoimmunotherapies that are administered in the neoadjuvant and adjuvant settings and will likely raise a new set of questions, including how much is enough.
Is neoadjuvant chemoimmunotherapy the new standard of care?
For N2-positive IIIA disease, I would say that neoadjuvant chemoimmunotherapy is absolutely the standard of care based on the results from CheckMate 816, and the safety data. The early pathologic responses are really impressive and are something we have never seen before. The pCR rate is one of the best predictive markers and we also now have evidence for improved event-free survival. So for N2 disease where outcomes are poor, this seems like a real improvement. Should it also be the standard of care for patients with N1 disease? I would think yes. In patients with resected N1 disease, the risk of recurrence is high, and I have always favored an induction pathway. I think having the primary tumor in place may help prime the immune system. Until we know otherwise, I think this hypothesis makes sense, because the science behind it looks good.
The more challenging question is, should it be standard of care in node-negative patients? There are node-negative patients with large primary tumors who meet the staging requirements to receive induction therapy. This is a major change in the way we deal with these patients. A patient may have a 4.5 cm peripheral tumor without nodal disease according to staging of the mediastinum. The standard approach for this patient has been upfront resection. A surgeon may see the patient on Tuesday, operate on Thursday, and the patient is home before Monday. Surgeons and patients both like this. The induction immunotherapy approach requires waiting for the biopsy results to rule out EGFR and ALK aberrations, which is followed by 9-12 weeks of therapy prior to resection. This represents a real change in the clinical care pathway and is especially difficult for surgeons with the approval of immunotherapy in the adjuvant setting. If data emerge in the next couple of years that show better survival with induction compared to an adjuvant approach, we will adapt our paradigm. But I think that changing care in patients with IB and II disease who are node-negative will be harder due to added steps than changing the care we provide for patients with IIIA or even IIB disease.
Which variables related to surgery itself are determinants of the success of curative surgery?
Twenty or 30 years ago, curative surgery meant removing the tumor with the patient staying alive. This is no longer enough, and many of the metrics that define a good operation are being refined. The increasing use of systemic therapy in earlier stages puts pressure on the surgeons to make their procedures as well tolerated as possible. In order for a patient to go on to adjuvant therapy within 4 weeks, the procedures need to go well and the patient needs to recover quickly. The Washington University group presented a great analysis at the ASCO Congress that assessed intraoperative quality metrics using very large databases [6]. Not surprisingly, the most important quality factor was R0 resection. If we leave tumor in the chest, we are doing our patients a disservice. Also, adequate nodal sampling is important. What qualifies as such is subject to constantly changing definitions, although thresholds of > 10 nodes or > 4 stations appear acceptable. Moreover, anatomic resections make a big difference.
These might be the most important metrics, next to timely and minimally invasive surgery. All of us need to work on our care pathways to make sure that patients move quickly from diagnosis to treatment. I always sit down with my patients prior to surgery and explain my priorities for each of them depending on age and fitness. Number 1 is of course not to put the patient’s life at risk. The next priority is to do a good oncologic operation and other priorities include saving lung tissue and keeping the procedure minimally invasive. These are the kind of quality discussions surgeons should have all the time. I think our quality metrics are going to become more important as we move into the era of effective adjuvant and neoadjuvant therapies.
Which biomarkers to guide therapy are currently on the rise?
At present, we are still struggling with biomarkers in lung cancer. PD-L1 expression has been in use, but we just saw data from the PEARLS/KEYNOTE-091 trial showing that the PD-L1 expression was not really helpful in predicting disease-free survival [7]. This was a little disconcerting. Many resected tumors undergo full genomic analysis, and we keep looking at things like STK-11 mutations in our attempt to identify a better biomarker out there. At the moment, tumor mutational burden does not quite appear to be the ideal marker, either. I think that new technologies like cell-free DNA are incredibly important. We have not been able to use this in early-stage lung cancer yet, because the platforms are not sensitive or reliable enough for patients without bulky stage III or stage IV disease, but this technology is advancing very quickly. I think that within the next 3 to 5 years, it will be good enough to give us an opportunity to escalate care in patients with earlier-stage lung cancer.
Figure: Proof-of-concept and further validation of neoadjuvant chemotherapy plus nivolumab
REFERENCES
- Provencio M et al., Neoadjuvant chemotherapy and nivolumab in resectable non-small-cell lung cancer (NADIM): an open-label, multicentre, single-arm, phase 2 trial. Lancet Oncol 2020; 21(11): 1413-1422
- Forde P et al., Neoadjuvant nivolumab plus chemotherapy in resectable lung cancer. New Engl J Med 2022; 386(21):1973-1985
- Spicer J et al., Surgical outcomes from the phase 3 CheckMate 816 trial: nivolumab + platinum- doublet chemotherapy vs. chemotherapy alone as neoadjuvant treatment for patients with resectable non-small cell lung cancer. J Clin Oncol 39, 2021 (suppl 15; abstr 8503)
- Provencio-Pulla M et al., Nivolumab + chemotherapy vs. CT as neoadjuvant treatment for resectable stage IIIA-B non-small cell lung cancer: NADIM II trial. J Clin Oncol 40, 2022 (suppl 16; abstr 8501)
- Qiu Fuming et al., Two cycles versus three cycles of neoadjuvant sintilimab plus platinum-doublet chemotherapy in patients with resectable non-small cell lung cancer (neoSCORE): a randomized, single center, two-arm phase II trial. J Clin Oncol 40, 2022 (suppl 16; abstr 8500)
- Heiden BT et al., Intraoperative quality metrics and association with survival following lung cancer resection. J Clin Oncol 40, 2022 (suppl 16; abstr 8502)
- O’Brien MO et al., EORTC-1416-LCG/ETOP 8-15 – PEARLS/KEYNOTE-091 study of pembrolizumab versus placebo for completely resected early-stage non-small cell lung cancer: outcomes in subgroups related to surgery, disease burden, and adjuvant chemotherapy use. J Clin Oncol 40, 2022 (suppl 16; abstr 8512)
© 2022 Springer-Verlag GmbH, Impressum