Combination of molecularly targeted drugs in lung cancer
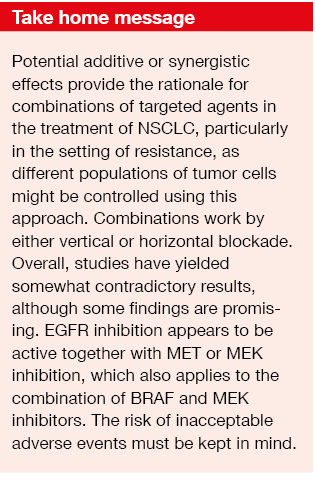
Most of the targeted agents currently recommended for the treatment of lung cancer are administered as single agents. However, there is a rationale for combinations, as two drugs might act in an additive or synergistic manner and may control different populations of tumor cells. Tumor heterogeneity plays a major role here, especially in patients who have already developed resistance to their first treatment.
Principles of evaluating combination regimens
Generally speaking, research into dual targeted inhibition in NSCLC patients has not yielded very successful results yet. If researchers plan to assess such an approach, it is important to create a strong scientific background portending the utility of a certain combination in order to avoid wasting time, money and effort. Pharmacological interactions must be kept in mind, as multiple pathways contribute to cell survival. Moreover, pharmacokinetic aspects (e.g., dose adjustments) deserve attention. The phase I is dedicated to working out the dose and feasibility of the combination. Here, the tests should demonstrate that the plasma level that is expected to inhibit the pathways is indeed achieved. Also, both drugs have to be shown to reach effective plasma concentrations. The phase II focuses on proving the clinical efficacy of the combination.
For phase III, there is a number of possibilities to evaluate dual targeted inhibition. Academic cancer groups need to work out if comparing A plus B to A or B is more useful than evaluating sequences of the two drugs. The focus of pharmaceutical companies will solely be on investigating the combination compared to the single agents. However, there is a rationale for sequences, as drugs can change the clonality and the tumor microenvironment, which might affect the activity of the subsequent treatment.
Resistance mechanisms in EGFR-mutant NSCLC
On the preclinical level, Huang et al. provided evidence that a two-drug combination with gefitinib and a MEK inhibitor might be used in acquired gefitinib resistance [1]. The MEK inhibitors AZD6244 (Figure 2) and CI-1040 were shown to reverse resistance in cells harboring EGFR mutations. These cells, as opposed to those with PC-9 wild type, have developed EGFR exon 19 deletion and thus have become anti-EGFR–resistant.
In addition, the NRAS Q61K mutation was identified in the gefitinib-resistant cells but not in those with PC-9 wild type. Although there are currently no NRAS-targeted agents available, MEK inhibition can be used as MEK is located downstream in the RAS/RAF/MEK pathway. A phase I/II study testing gefitinib plus the MEK 1/2 inhibitor selumetinib is ongoing in EGFR-TKI–resistant patients with EGFR T790M mutation.
Figure 2: Reversal of gefitinib resistance in PC-9 cells using the MEK inhibitor AZD6244.
Modified from Huang MH et al. [1]
cMET plus EGFR inhibition
EGFR inhibition combined with MEK inhibition is an example of a vertical blockade. The horizontal blockade, on the other hand, relates to the inhibition of two pathways that both independently trigger the same signal transduction cascade. An example of a horizontal blockade is MET inhibition in combination with EGFR inhibition in acquired EGFR TKI resistance. MET amplification occurs in approximately 20 % of erlotinib- or gefitinib-treated NSCLC patients, and in approximately 5 % of erlotinib/ gefitinib-naïve patients [2]. In gefitinib-resistant HCC827 cells, both EGFR and MET inhibition are required to induce apoptosis.
Another study confirmed that resistance does not come alone. Patients with EGFR T790M mutation sometimes also display MET amplification and vice versa, which complicates the picture [3]. Patients with the T790M mutation will not respond if gefitinib is added to a MET inhibitor. Overexpression of the hepatocyte growth factor, which is a MET ligand, also contributes to EGFR TKI resistance. These patients might benefit from a MET inhibitor that is administered along with EGFR TKI therapy.
Preliminary clinical data from the phase Ib expansion cohort of the TATTON trial suggest encouraging activity of the EGFR TKI osimertinib combined with the MET inhibitor savolitinib in patients with EGFR-mutation–positive, MET-positive NSCLC [4]. The response rates ranged from 33 % to 61 %. However, the possibility of adverse events must be kept in mind. Another arm of the TATTON trial evaluated osimertinib in combination with the checkpoint inhibitor durvalumab, and this regimen led to inacceptable rates of interstitial lung fibrosis [5]. The lung changes occurred with a considerable delay after the end of the study, and the phase III trial that was already ongoing had to be terminated.
Results obtained with INC280
The investigational oral MET inhibitor INC280 was tested together with gefitinib in patients with EGFR-mutant, MET-amplified NSCLC progressing on EGFR TKI treatment [6]. In this phase Ib/II, open-label, multicenter study, molecular pre-screening identified patients with MET dysregulation who had developed resistance to gefitinib or erlotinib. Thirty-eight patients were included in the phase II of the trial; they responded well to the treatment with INC280 plus gefitinib (Figure 3).
These patients had not been tested for the EGFR T790M mutation, but it can be assumed that they were not T790M-positive, as otherwise they would not have responded. Pronounced MET amplification or high MET protein expression might preclude the presence of T790M, although further study into this is required.
Figure 3: Tumor responses to INC280 plus gefitinib in patients with EGFR-mutant, gefitinib-resistant, MET-positive NSCLC. Modified from Wu Y-L et al. [6]
BRAF alterations
Although BRAF inhibition works well in patients with melanoma, single-agent dabrafenib therapy gave rise to a surprisingly low response rate (RR) of 33 % in patients with BRAFV600E-mutant metastatic NSCLC participating in a multi-center, open-label phase II trial [7]. RRs achieved with the blockage of a genuine driver mutation are expected to range between 50 % and 70 %.
As for patients with melanoma, the combined approach using both BRAF and MEK inhibition, which induces vertical blockade, was shown to yield improved results in the NSCLC setting. A phase II trial investigating dabrafenib plus trametinib revealed an RR of 63 %, and disease control occurred in 79 % [8]. Also, PFS was longer with the combination than with dabrafenib alone (9.7 vs. 5.5 months). The rationale behind the addition of a MEK inhibitor is based on the observation that compensatory over-activation of downstream MEK ensues when a BRAF inhibitor is administered [9-13]. Early resistance and skin cancer can occur. These effects are prevented by the use of the combination.
Unexplained phenomena
Not all of the targeted agents can be combined, however, and the analysis of combinations does not always reveal predictable results. For instance, erlotinib plus cetuximab evoked no responses whatsoever in a trial setting aimed to overcome acquired resistance to anti-EGFR treatment [14]. On the other hand, data obtained in the mouse model showed activity of afatinib plus cetuximab regardless of the presence of the EGFR T790M mutation [15]. A variety of anticancer agents was tested here, but only this combination induced dramatic shrinkage of erlotinib-resistant tumors. The authors noted that afatinib and cetuximab jointly depleted both phosphorylated and total EGFR in an efficient manner.
These observations are actually unexplained against the background of the current knowledge of molecular pathways. The synergistic effect of a TKI and an antibody cannot be due to vertical or horizontal blockade. One of the hypotheses relating to this phenomenon states that once the extracellular domain binds to the antibody, the tyrosine kinase conformation will change. However, there is currently no way to assess conformational changes. Another theory refers to the fact that homodimerisation is not symmetric but rather asymmetric. TKIs only exert their effects by binding to one part of the EGFR, which means that binding must occur at the correct side of the tyrosine kinase [16]. If the drug binds at the inactive site, it will not show any activity.
Nevertheless, the interest in combination therapy has been renewed due to the issue of osimertinib resistance, as there is no targeted therapy available for these patients. The experiences described above illustrate how little is actually known at present.
REFERENCES
- Huang MH et al., MEK inhibitors reverse resistance in epidermal growth factor receptor mutation lung cancer cells with acquired resistance to gefitinib. Mol Onco 2013; 7(1): 112-120
- Engelman JA et al., MET amplification leads to gefitinib resistance in lung cancer by activating ERBB3 signaling. Science 2007; v316(5827): v1039-v1043
- Bean J et al., MET amplification occurs with or without T790M mutations in EGFR mutant lung tumors with acquired resistance to gefitinib or erlotinib. Proc Natl Acad Sci U S A 2007; 104(52): 20932-20937
- Ahn MJ et al., TATTON phase Ib expansion cohort: osimertinib plus savolitinib for patients with EGFR-mutant MET-amplified NSCLC after progression on prior EGFR-TKI. WCLC 2017, OA 09.03
- Ahn MJ et al., Osimertinib combined with durvalumab in EGFR-mutant non-small cell lung cancer: results from the TATTON phase Ib trial. J Thorac Oncol 2016; 11(4 Suppl): S115
- Wu Y-L et al., Phase (Ph) II safety and efficacy results of a single-arm ph Ib/II study of capmatinib (INC280) + gefitinib in patients (pts) with EGFR-mutated (mut), cMET-positive (cMET+) non-small cell lung cancer. J Clin Oncol 2016; 34: abstract 9020
- Planchard D et al., Dabrafenib in patients with BRAF(V600E)-positive advanced non-small-cell lung cancer: a single-arm, multicentre, open-label, phase 2 trial. Lancet Oncol 2016; 17(5): 642-650
- Planchard D et al., Dabrafenib plus trametinib in patients with previously treated BRAFV600E-mutant metastatic non-small cell lung cancer: an open-label, multicenter phase 2 trial. Lancet Oncol 2017; 18(10): 1307-1316
- Davies H et al., Mutations of the BRAF gene in human cancer. Nature 2002; 417(6892): 949-954
- Platz A et al., Human cutaneous melanoma; a review of NRAS and BRAF mutation frequencies in relation to histogenetic subclass and body site. Mol Oncol 2008; 1(4): 395-405
- Karasarides M et al., B-RAF is a therapeutic target in melanoma. Oncogene 2004; 23(37): 6292-6298
- Long GV et al., Combined BRAF and MEK inhibition versus BRAF inhibition alone in melanoma. N Engl J Med 2014; 371(20): 1877-1888
- Gilmartin AG et al., GSK1120212 (JTP-74057) is an inhibitor of MEK activity and activation with favorable pharmacokinetic properties for sustained in vivo pathway inhibition. Clin Cancer Res 2011; 17(5): 989-1000
- Janjigian YY et al., Phase I/II trial of cetuximab and erlotinib in patients with lung adenocarcinoma and acquired resistance to erlotinib. Clin Cancer Res 2011; 17(8): 2521-2527
- Regales L et al., Dual targeting of EGFR can overcome a major drug resistance mutation in mouse models of EGFR mutant lung cancer. J Clin Invest 2009; 119(10): 3000-3010
- Jura N et al., Mechanism for activation of the EGF receptor catalytic domain by the juxtamembrane segment. Cell 2009; 137(7): 1293-1307
Content based on an young oncology preceptorship conducted by JSMO on 8th–10th December 2017 in Singapore, with an unrestricted grant from Boehringer Ingelheim


![Figure 2: Reversal of gefitinib resistance in PC-9 cells using the MEK inhibitor AZD6244. Modified from Huang MH et al. [1]](https://memoinoncology.com/wp-content/uploads/2020/04/Grafik-8-preceptorship-singapore-en.png)
![Figure 3: Tumor responses to INC280 plus gefitinib in patients with EGFR-mutant, gefitinib-resistant, MET-positive NSCLC. Modified from Wu Y-L et al. [6]](https://memoinoncology.com/wp-content/uploads/2020/04/Grafik-9-preceptorship-singapore-en.png)