Novel bispecific antibodies in CD20-positive B-cell non-Hodgkin lymphomas
Glofitamab step-up dosing
The T-cell–engaging bispecific antibody glofitamab has been designed with a 2:1 configuration that enables bivalent binding to CD20 on B cells and monovalent binding to CD3 on T cells [1]. Compared to alternative bispecific formats, this offers greater avidity, potency and combinability with other anti-CD20 IgG antibodies. In the phase I setting, glofitamab step-up dosing after obinutuzumab pretreatment allowed for dose escalation of up to 30 mg to maximize efficacy while mitigating the cytokine release syndrome (CRS) risk [2]. At ICML 2021, Carlo-Stella et al. presented updated efficacy data for two cohorts (including the final, recommended phase II dose) from the ongoing phase I/II dose escalation and expansion study conducted in patients with relapsed/refractory non-Hodgkin lymphoma (NHL) [3].
In these cohorts, glofitamab was administered intravenously in step-up doses of 2.5 mg and 10 mg on days 1 and 8 of cycle 1, respectively, followed by two different target doses of 16 mg or 30 mg from day 1 of cycle 2. After cycle 1, which encompassed 14 days, glofitamab was given 3-weekly for up to twelve cycles. Obinutuzumab pretreatment was administered seven days prior to glofitamab therapy. Among 50 patients with CD20-expressing B-cell NHLs, 16 and 34, respectively, were assigned to the 2.5/10/16 mg and 2.5/10/30 mg schedules. Most patients were heavily pretreated; the median number of prior lines was 3, and 84.6 % were refractory to any prior therapy. All patients had received prior chemotherapy and anti-CD20 antibody therapy. Aggressive and indolent NHLs were present in 53.8 % and 46.2 %, respectively. Diffuse large B-cell lymphoma (DLBCL) was the most common aggressive entity. All patients with indolent NHL had follicular lymphoma (FL) grade 1-3a.
Durable CMRs
The update of the study revealed high response rates. Overall, 64.3 % and 79.2 % of patients with aggressive and indolent disease, respectively, responded. Those with aggressive NHLs receiving the 2.5/10/30 mg dose showed a trend, with a complete metabolic response (CMR) rate of 71.4 %. Four of five patients with mantle cell lymphoma (MCL) achieved CMR. The majority of patients experienced at least 50 % reductions in tumor burden, with anti-tumor activity evident across NHL subtypes.
The median duration of response for complete responders had not been reached after a median follow-up of 8.4 and 5.8 months for aggressive and indolent NHLs, respectively. In the group with aggressive lymphomas, 13 out of 16 CMRs were shown to be ongoing at the time of the analysis, and for indolent lymphomas, 16 of 17 CMRs were ongoing. Most patients in the entire population receiving the 2.5/10/30 mg schedule experienced significant durability of CMR even after treatment completion. Moreover, immunohistochemistry and immunofluorescence analysis of baseline tumor biopsies demonstrated that clinical responses were achieved across a range of CD20 expression levels and irrespective of the amount of tumor infiltration by CD8 T-cells.
Adverse events (AEs) mainly included CRS, neutropenia, and pyrexia. CRS events emerged in 67.3 % of patients, but they were confined to the first two cycles and were graded as 1 or 2 in the vast majority of cases (grade 1, 38.5 %; grade 2, 23.1 %). Glofitamab doses of 2.5 mg and 10 mg administered in cycle 1 gave rise to CRS rates of 48.0 % and 40.8 %, respectively. In cycle 2, 12.4 % and 30.3 % of patients receiving 16 mg and 30 mg, respectively, developed CRS. Grade 3 CRS events were restricted to 3.8 % of patients treated with 30 mg in cycle 2. Overall, treatment-related grade 3/4 AEs occurred in 40.4 %. No grade 5 AEs were reported. Treatment discontinuation resulting from AEs was seen in 3.8 %. The authors noted in their conclusions that these glofitamab step-up dosing data showed impressive response rates, potentially translating into early and more durable responses for patients with aggressive and indolent relapsed/refractory NHL who have failed multiple lines of therapy.
Epcoritamab: EPCORETM NHL-1
Similar to glofitamab, epcoritamab is a bispecific antibody that binds CD20 and CD3, which harnesses the patient’s immune system to induce T-cell–mediated killing of CD20-positive malignant B-cells [4]. However, epcoritamab is administered subcutaneously, thus ensuring more gradual increases and lower peaks in plasma cytokine levels compared to intravenous formulations, and this is regarded as a strategy to mitigate CRS. Other features include an ability for potent T-cell–mediated killing even at low levels of CD20 expression, as well as Fc domain mutations that prevent off-target T-cell cytotoxicity.
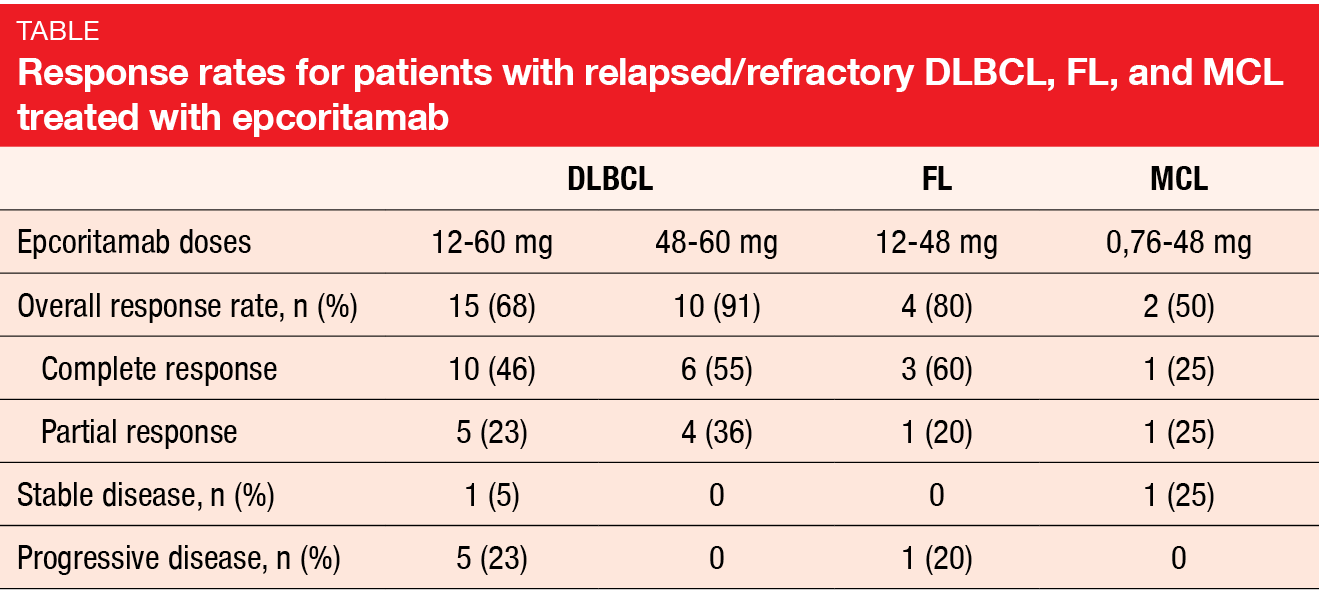
The dose-escalation part of the ongoing, first-in-human phase I/II EPCORETM NHL-1 study has identified 48 mg as the recommended phase II dose in patients with relapsed/refractory CD20-positive B-NHL previously treated with anti-CD20 antibodies [5]. No dose-limiting toxicities were observed, and the maximum tolerated dose was not reached. Patients are currently being treated in the expansion cohort. Hutchings et al. reported updated data for 68 patients after a median follow-up of 14.1 months at ICML 2021 [6]. The majority had DLBCL (n = 46), followed by FL and MCL. Most of them were heavily pretreated and refractory to their most recent line of therapy, as well as to prior anti-CD20 combinations.
Encouraging activity
Despite these unfavorable prerequisites, epcoritamab demonstrated encouraging anti-tumor activity with deep responses across histologies. Among DLBCL patients who received 48–60 mg, the ORR was 91 %, with 55 % achieving complete remission (CR; Table). For patients with FL, this was 80 % and 60 %, respectively. Responses were obtained in all five DLBCL patients previously treated with CAR-T cell therapy. In the entire cohort, median time to response was 1.3–1.9 months across dose groups, and median duration of response had not been reached yet. All DLBCL patients who achieved CR with ≥ 12 mg doses have remained in remission; three of them went on to receive consolidation stem cell transplantation. Median progression-free survival was 9.1 month for those treated with ≥ 12 mg, while it had not been reached yet in the ≥ 48 mg dose group. Four of five FL patients who achieved CR with ≥ 0.76 mg doses remained in remission at a median follow-up of 11.1 months.
Epcoritamab was generally well tolerated. Most commonly, pyrexia (69 %) and CRS (59 %) occurred, followed by injection site reaction (47 %), fatigue (44 %), hypotension (31 %), diarrhea (26 %), dyspnea (25 %), anemia (23 %), and tachycardia (21 %). The safety profile was consistent across doses and histologies, and the majority of AEs were mild or moderate. Notably, no grade ≥ 3 CRS events were observed, and grade 1/2 events resolved with standard-of-care management. Almost all CRS events were restricted to cycle 1. The risk of CRS was mitigated by the subcutaneous administration, step-up dosing and corticosteroid prophylaxis during cycle 1. Neurotoxicity was rare, self-limiting and transient. No treatment-related deaths or discontinuations occurred.
The expansion part of the EPCORETM NHL-1 study is ongoing. Furthermore, epcoritamb is currently being studied in the phase III EPCORETM DLBCL-1 trial as monotherapy versus standard-of-care chemotherapy in patients with relapsed/refractory DLBCL, as well as in phase I/II trials across different B-cell NHL histologies, and in various combinations and settings.
REFERENCES
- Bacac M et al., CD20-TCB with obinutuzumab pretreatment as next-generation treatment of hematologic malignancies. Clin Cancer Res 2018; 24: 4785-4797
- Hutchings M et al., Glofitamab, a novel, bivalent CD20-targeting T-cell–engaging bispecific antibody, induces durable complete remissions in relapsed or refractory B-cell lymphoma: a phase I trial. J Clin Oncol 2021; 39(18): 1959-1970
- Carlo-Stella C et al., Glofitamab step-up dosing: updated efficacy data show high complete response rates in heavily pretreated relapsed/refractory non-Hodgkin lymphoma patients. ICML 2021, 015
- Engelberts PJ et al., DuoBody-CD3xCD20 induces potent T-cell-mediated killing of malignant B cells in preclinical models and provides opportunities for subcutaneous dosing. EBioMedicine 2020; 52: 102625
- Hutchings M et al., Subcutaneous epcoritamab induces complete responses with an encouraging safety profile across relapsed/refractory B-cell non-Hodgkin lymphoma subtypes, including patients with prior CAR-T therapy: updated dose escalation data. ASH 2020, 402
- Hutchings M et al., Subcutaneous epcoritamab in patients with relapsed/refractory B-cell non-Hodgkin lymphoma: safety profile and anti-tumor activity. ICML 2021, 016
© 2021 Springer-Verlag GmbH, Impressum
More posts
Zanubrutinib in relapsed/refractory marginal zone lymphoma: MAGNOLIA
Zanubrutinib in relapsed/refractory marginal zone lymphoma: MAGNOLIA B-cell rec
Mantle cell lymphoma: improving outcomes in difficult-to-treat patient populations
Mantle cell lymphoma: improving outcomes in difficult-to-treat patient populations
Extending anti-PD-1–based options in the setting of Hodgkin lymphoma
Extending anti-PD-1–based options in the setting of Hodgkin lymphoma Patients w
Successful inhibition of PI3K, BTK, BCL2 and other targets in various B-cell malignancies
Successful inhibition of PI3K, BTK, BCL2 and other targets in various B-cell malign
Waldenström’s macroglobulinemia: outcome optimization via combinations
Waldenström’s macroglobulinemia: outcome optimization via combinations Final an
CLL/SLL: current perspectives across a range of potent agents
CLL/SLL: current perspectives across a range of potent agents ALPINE: zanubruti